Childhood cancer advocate, speaker, and bestselling author of The Cancer Parent’s Handbook: What Your Oncologist Doesn’t Have Time to Tell You
Reality Check
Let’s get real for a minute. Throughout treatment, didn’t you dream about the finish line and how amazing it would feel if you were lucky enough to get there? Your heroic comeback, the day you finally get your “old life” back? As the caregiver of an ALL survivor, I sure did.
I thought that once my daughter Cecilia’s cancer was in remission, I would be filled with relief, gratitude, and joy. Certainly, when she was nearing the end of her two-and-a-half years of treatment, I would be cartwheeling, walking on water. Right?
Yes, there were joyful moments of anticipation for the finish line. But if I’m being honest, most of the time all I felt was fear. Pesky, sometimes debilitating, looking-over-your-shoulder fear.
Because here’s what nobody tells you in the beginning: wrapping up treatment isn’t the end of the journey. It’s a step. There are follow-up tests, some potential fear around stopping chemo and radiation (so ironic considering how much you dreaded it), and if you are a caregiver, it can be unsettling to be ‘done’ and without a job. The emotional rollercoaster is real, and for most of us, it sneaks up at a time when we only expected to feel relief.
If you’re reading this, you (or your child or loved one) ran a marathon. Now, as a Survivor, it’s time to reset. Time to care for yourself in a completely new way, honoring the trauma you’ve been through while celebrating how amazing it is that you are done with treatment. This article and the accompanying resources from CAC2 are your reset guide, loaded with the practical tools, tricks, and compassion I needed and collected during our journey, and used to create my bestselling book The Cancer Parent’s Handbook ~What Your Oncologist Doesn’t Have Time to Tell You.
Why the “End of Treatment” Might Not Feel Like the “End”
Once the daily chemo, endless pokes and procedures, and doctors fade away, you’d think your mind and body would simply slide into a chill state. While there are exceptions, generally it’s a bit more complicated than that. Yes! There is joy in finishing treatment for sure. But here’s the reality: trauma, stress, and those endless months of fight-or-flight mode leave us wired for danger long after the crisis ends unless we take action. Insomnia, panic, negative spiraling… all of these are normal when we live in fight-or-flight mode. They aren’t signs of weakness; this is how your body protects you and warns you that you need some help. But we are not meant to live this way for extended periods of time.
Medical trauma, whether you’re the one who endured it, or the caregiver, kicks up our animal instinct. A certain smell, a song, a date on the calendar, or an innocent question from a friend can send your heart racing and your mind into a negative spiral. It’s not just “in your head”, it’s a whole body event too.
So, what can you do?
You build yourself a post-treatment toolkit, using ideas from this article and the resources associated with this CAC2 section. Let’s get to it.
Tools to Reset Your Mind & Body
Trauma doesn’t just live in our memories, it also shows up in our bodies, as tension, pain, or
other symptoms. When we notice these physical signs, it’s natural for our minds to react,
whether through emotions, worries, or memories. This is a normal part of how our bodies and minds work together to process difficult experiences.
“Trauma is not just an event that took place in the past;
it is also the imprint left by that experience on mind, brain, and body.”
– Bessel van der Kolk, M.D., The Body Keeps the Score
Below are 10 tried and true strategies that helped me, my daughter, and so many families I’ve walked alongside during treatment and while writing The Cancer Parent’s Handbook: gentle and practical steps that soothe both body and mind. Small things you can do, even in the hardest moments, to find a little more calm, connection, and hope as you transition into
survivorship.

Name It
First, when unexplained anxiety or stress hits, name what’s happening to you without judging it. Instead of feeling like you are spiraling yet again, say to yourself: “This is a trauma response.” The minute you do, you take back a little control. It’s not you being “dramatic,” it’s your body trying to do its job.
Ground Yourself
Survivors and caregivers become used to living in a tense state, and we need help on the other side of treatment to feel more centered in life. A concept professionals call ‘Grounding’ can be very helpful. There are several aspects to Grounding that we have included in the CAC2 resources section, including:
● Walking barefoot at the beach or on grass
● Circular breathing
● Cool therapy
● Yoga
● Meditation
Grounding is a cornerstone of trauma-conscious, practical healing. According to experts, Grounding techniques are not simply distractions when you are uncomfortable, they reset your body and mind. By drawing our awareness to what’s happening in our bodies and senses right now through walking on the earth, breathing practices, etc., we gently shift ourselves out of loops of distress, anxiety, or dissociation. In these small, purposeful moments, we rediscover agency and find a foothold for calming ourselves down at any time.
Toolkit Tip: Check YouTube where you’ll find lots of free classes for mind and body, from breathing practices to meditation and gentle yoga. You’ll find things for yourself, your child, or loved ones that can make a difference and they are often free!
For those of us who have been through a lot, cool water works better than heat or cold water in calming our nervous system. Heat ramps up that hot, flushed, trapped feeling that panic brings, and cold can stress out our nervous system. Cool water slows everything down, eases that wired sensation, and makes it much easier to get a grip and move forward.
Exercise and Nutrition
Exercise and good nutrition are foundational for getting stronger after treatment, and it doesn’t have to be complicated. Just moving your body can help you reset when emotions go on overload. I’ve power-walked hospital corridors more times than I can count, sometimes just to keep from crying, or after a tough conversation with a doctor or even after a meeting at work that didn’t go as planned. Taking a moment to breathe and move gives you space to figure out your next step, even if that step is… nothing.
If working out is your thing, great! Get back into your gym routine, but start slowly. Your body’s been through a lot, and pushing too hard can backfire.
Fuel that beautiful body with protein, leafy greens, and healthy carbs. You’ve heard it a million times, but it’s true. Check out our Resources section, clean out your pantry, and remember what your body has done for you.
Breathe
Breathwork is a highly effective tool you can use both during treatment for things like needle sticks or anxiety-provoking procedures, and after treatment when unpleasant feelings or memories hit, or even during a heated business meeting.
There are many options, but Box Breathing is a popular choice for regulating your nervous system:
Inhale for 4, hold for 4, exhale for 4, hold for 4. Repeat four times for maximum effect.
Toolkit Tip:
When you are bogged down with negative thoughts, sing out loud or hum your favorite songs. The vibrations tell your body that you are safe. And it’s a mood lifter!
Create Rituals
I cannot overstate how powerful it is to have a ritual every day that centers you, especially when you are recovering from trauma. I started a quiet, no-talking, no-phone morning routine with tea and a short spiritual reading during treatment. At night, I kept a gratitude journal. I still do both to this day. For my daughter, it was daily journaling and meditation to work through her post-treatment anger.
Your ritual can be anything that gets you off your phone and out of your head. Guard those moments fiercely (no interruptions!) as it’s sacred time. Consistency is key.
Body-Based Healing
Since trauma lives in the body, modalities such as acupuncture, massage, restorative yoga, or even just lying in the grass help tame the storm. Turn to the CAC2 resource list for how to find low-cost or free support in all of these areas. All are incredibly helpful in restoring mind and body.
Toolkit Tip:
If you have a local massage school, check out their website to find out their prices for student massages. At my local place, Cypress Massage, a 90-minute deep tissue massage by a trained student is $25! Such a deal!
Write it Out
There are a few ways that writing can help you process trauma. Two that have been particularly powerful to me and my family are Morning Pages and a Gratitude Journal.
Morning Pages:
Set aside at least 15 minutes a day—or whenever you feel the need—for Morning Pages. Here’s how it works: Before your day gets underway, sit down with your coffee or tea and “worry out loud” on paper. No holding back, no editing, no making it pretty. Just write whatever’s on your mind. When you’re finished, tear up or toss the pages. Morning Pages are a powerful way to let go of worries, quiet your mind, and break the cycle of recurring negative thoughts.
Gratitude Journal:
At the end of each day, take a moment to write down five good things that happened. Keep it simple—a yummy breakfast, a fun text with a friend, or seeing a glorious sunset. This small ritual gently trains your mind to notice the tiny joys that appear even the hardest days. Over time, it helps shift your focus, giving you a sense of calm and hope when anxiety creeps in. When you see the good laid out on the page, it becomes a little easier to believe that your day was good, maybe even great. And the reassurance that more joy can be found tomorrow.
If you remember nothing else, remember this:
Whether you’re the patient or the caregiver, you did something incredibly hard. And you’re still doing it! Cancer treatment takes a toll, and even long after the last dose, the last scan, the last sleepless night, triggers will happen. Let them flow through you, breathe, and remind yourself: it’s just a thought, not reality.
And if you can’t shake the negativity off or get unstuck, seek help. Talk to someone who’s trained in trauma therapy and process this journey and your understandable grief. Asking for support isn’t a failure; it’s one of the strongest, bravest moves you can make.
Healing isn’t linear and doesn’t follow a predictable schedule. So stay in practice and make space to focus on yourself every day.
You’re not alone. I’ve got you.
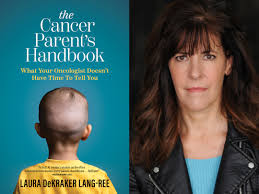
I wrote The Cancer Parent’s Handbook: What Your Oncologist Doesn’t Have Time to Tell You to be the guide I needed when my daughter was diagnosed. It’s full of real talk, practical tips, and honest support on everything from hospital life and sibling dynamics to asking for help and becoming your child’s best advocate. You’ll find more on this topic—and much more—at my website.
Laura DeKraker Lang-Ree